Autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic or inherited disease of the kidney, characterized by the growth of numerous cysts in the kidneys. Polycystic kidney disease (PKD) is the fourth leading cause of chronic kidney disease. In PKD, other organs in which cysts can be seen are the liver, brain, intestines, pancreas, ovaries and spleen.
What is the incidence of PKD?
 The incidence of autosomal dominant PKD is the same in all races, occurs equally in males and females and affects about 1 in 1,000 people worldwide. About 5% of all chronic kidney disease patients requiring dialysis or kidney transplantation have PKD.
The incidence of autosomal dominant PKD is the same in all races, occurs equally in males and females and affects about 1 in 1,000 people worldwide. About 5% of all chronic kidney disease patients requiring dialysis or kidney transplantation have PKD.
How is the kidney affected in PKD?
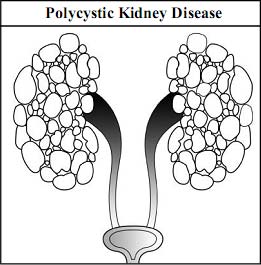
In autosomal dominant PKD multiple clusters of cysts (fluid-filled sacs) are seen in both kidneys.
Sizes of cysts in PKD are variable (diameter ranging from a pinhead to as large 10 cm. or more). With time cysts increase in size and slowly compress and damage healthy kidney tissue.
Such damage leads to hypertension, loss of protein in urine and reduction in kidney function, causing chronic kidney failure.
In a long period (after years) chronic kidney failure worsens and leads to severe kidney failure (endstage kidney disease), ultimately requiring dialysis or kidney transplantation.
Symptoms of PKD
Many people with autosomal dominant PKD live for several decades without developing symptoms. Most patients with PKD develop symptoms after the age of 30 to 40 years. Common symptoms of PKD are:
- High blood pressure.
- Pain in the back, flank pain on one or both sides and/or a swollen abdomen.
- Feeling a large mass (lump) in abdomen.
- Blood or protein in urine.
- Recurrent urinary tract infections and kidney stones.
- Symptoms of chronic kidney disease due to progressive loss of kidney function.
- Symptoms due to cysts in other parts of the body such as the brain, liver, intestine.
- Complications that can occur in a patient with PKD are brain aneurysm, abdominal wall hernias, infection of liver cysts, diverticulae (pouches) in the colon and heart valve abnormalities. About 10% of PKD patients develop a brain aneurysm. An aneurysm is a weakeningof the wall of the blood vessel which causes bulging. Brain aneurysms can cause headaches and carry a small risk of rupture that can lead to a stroke or even death.
PKD is the most commonly inherited kidney disease and among the leading causes of CKD.
Does everyone with PKD develop kidney failure?
No. Kidney failure does not occur in all patients with PKD. About 50 % of patients with PKD will have kidney failure by the age of 60, and about 60 % will have kidney failure by the age of 70. The risk factors for progression of CKD in patients with PKD include: larger renal size, younger age at diagnosis, hypertension (particularly before age 35 years), proteinuria (> 300 mgs/day), gross hematuria, male gender, > 3 pregnancies, certain genetic mutations (PKD1 gene mutation), as well as tobacco consumption.
Diagnosis of PKD
Diagnostic tests performed in autosomal dominant PKD are:
- Ultrasound of the kidneys. This is the most commonly used diagnostic test for PKD because it is reliable, simple, safe, painless, less costly, and easily identifies cysts in the kidneys.
- CT or MRI scans: These tests are more precise but are expensive. These tests may detect smaller cysts that cannot be diagnosed by an ultrasound.
- Family screening: PKD is an inherited disease in which each child has a 50:50 chance of developing the disease. So screening of family members of a patient with PKD helps in early diagnosis.
- Tests to assess effect of PKD on kidney: Urine test is done to detect the presence of blood or protein in urine. Blood test for creatinine is done to assess and monitor the function of the kidney.
- Incidental diagnosis: PKD detected in routine health check up or during ultrasound examination done for another reason.
- Gene linkage analysis: This is a very specialized blood test, used to detect which family member carries the PKD gene. This test should be done only if imaging tests do not show anything. As this test is available in very few centers and is very expensive, it is done rarely for diagnostic purposes.
Which family members of PKD patients should be screened for PKD?
Brothers, sisters and children of PKD patients should be screened for PKD. In addition, brothers and sisters of parents from whom the disease is inherited by the patient should be screened.
Will all children of PKD patients carry the risk of developing the same disease?
No. PKD is an inherited disease in which if mother or father has autosomal dominant PKD, the children have a 50% possibility of developing the disorder.
Flank and abdominal pain and blood in urine at the age of 40 is the most common presentation of PKD.
Prevention of PKD
Currently there is no treatment that can prevent formation or slow down the growth of cysts in PKD.
Screening of family members and making an early diagnosis before it sets in has several advantages. Early diagnosis provides an opportunity to treat PKD in a better way. Early diagnosis and treatment of high blood pressure prevents development or aggravation of renal failure in PKD. Lifestyle and dietary modification in PKD patients protects their kidney as well as the heart. The major disadvantage of screening is that the person may become very anxious about the disease at a stage when the person neither has the symptoms nor needs any treatment.
PKD is an inherited kidney disease so consider screening of adult family members for PKD.
Why is it not possible to reduce the incidence of PKD?
PKD is diagnosed usually at the age of 40 years or more. Most people have children before this age and therefore it is not possible to prevent its transmission to the next generation.
Treatment of PKD
PKD is a non-curable disease but why does it need treatment?
- To protect the kidneys and delay progression of chronic kidney disease to end stage kidney disease and thereby prolong survival.
- To control the symptoms and prevent complications.
Important measures in the treatment of PKD:
- The patient is asymptomatic for many years after initial diagnosis and does not require any treatment. Such patients need periodic checkup and monitoring.
- Strict control of high blood pressure will slow down the progression of CKD.
- Control of pain with drugs which will not harm the kidney (such as aspirin or acetaminophen). Recurrent or chronic pain occurs in PKD due to cyst expansion.
- Prompt and adequate treatment of urinary tract infections with appropriate antibiotics.
- Early treatment of kidney stones.
- Plenty of fluid intake, provided the person does not have swelling helps in prevention of urinary tract infections and kidney stones.
- Meticulous treatment of chronic kidney disease as discussed in Chapters 10 to 14.
- In a very few patients surgical or radiologic drainage of cysts may be indicated because of pain, bleeding, infection, or obstruction.
Treatment is aimed at delaying progression of CKD and treating kidney infections, stones and abdominal pain.
When should a patient with PKD consult a doctor?
Patients with PKD should immediately consult a doctor if he or she develops:
- Fever, sudden abdominal pain or red urine.
- Severe or recurrent headaches.
- Accidental injury to enlarged kidneys.
- Chest pain, severe loss of appetite, severe vomiting, severe muscle weakness, confusion, drowsiness, unconsciousness or convulsion.
Asymptomatic person with PKD may not require any treatment for many years initially.